
Over recent years, mindfulness-based interventions (MBIs) have gained attention as powerful tools for supporting people living with long-term health conditions—including Multiple Sclerosis (MS). For people with MS (PwMS), the journey is often marked by unpredictability, physical and cognitive loss of function, and significant changes in self-identity.

Yvette Sargood and Phil Startin are two mindfulness teachers who have each lived with MS for over 15 years. They’ve seen firsthand how mindfulness can help navigate this terrain. In this blog, we explore how mindfulness supports those with MS, what adaptations make MBIs more accessible, and the powerful outcomes many experience through practice.
Understanding MS and Its Impact
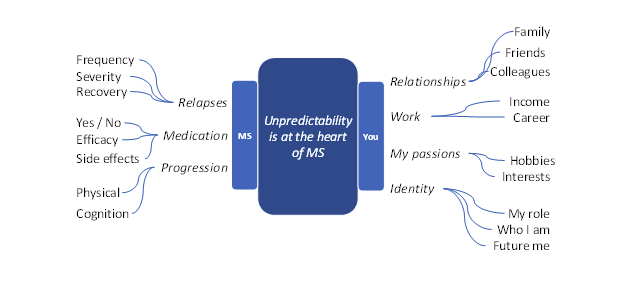
MS is a chronic, inflammatory, and degenerative condition of the central nervous system that affects over 2.9 million people worldwide. Symptoms vary widely, but one shared experience is the unpredictability regarding the future course of the condition and its impact on health and identity.
This unpredictability can trigger anxiety, stress, and feelings of helplessness or loss of control. Many PwMS ask: What will happen next? Will I lose mobility? How will this affect who I am? Mindfulness helps individuals face these challenges not by removing uncertainty, but by changing their relationship to it.
Common Reactions to MS
From our personal experience and teaching—delivering 18 mindfulness courses to over 150 PwMS—we’ve observed that people with MS often struggle with:
· Fear of the future and catastrophising
· Shame or isolation, believing “it’s just me”
· Rumination and longing for the way things used to be
· Loss of identity, especially when abilities or roles change
These reactions are natural—but they can become obstacles to well-being if left unchecked. As stress plays a role in the progression of MS, such reactions may even exacerbate the condition, which in turn can generate more stress—creating a vicious circle that adds to the sense of helplessness. Research also suggests that MS itself may cause physical changes in the brain that contribute to depression and anxiety.
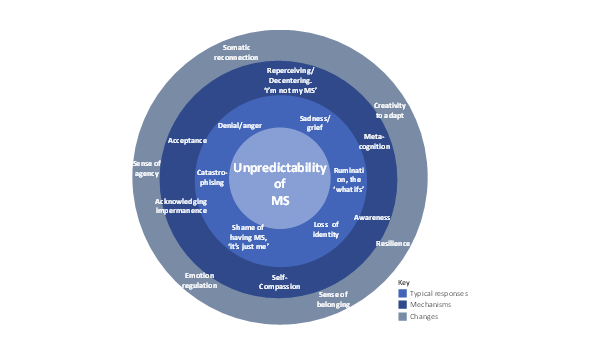
To better understand and communicate how mindfulness can help, we created the Mindfulness and Self-Compassion Model for MS (Sargood & Startin, 2025. Above)
The model places the unpredictability of MS at its centre, with outer rings showing typical responses—such as fear, shame, and disconnection—as well as the mechanisms we’ve observed and the ways mindfulness and self-compassion can support change.
Mindfulness: A New Way to Relate
For PwMS, mindfulness offers a new way to relate to thoughts, emotions, the body, and the ongoing changes brought by the condition. It supports:
Holding Thoughts and Emotions More Lightly: PwMS often spiral into “what if” thinking. Mindfulness builds meta-cognition—awareness that thoughts are just thoughts—which helps reduce anxiety and interrupt unhelpful patterns.
Reconnecting with the Body: Pain, discomfort and loss of function can lead to disconnection from the body. Somatic practices like body scans encourage gentle reconnection, shifting from judgment to compassion, and noticing the body with care rather than criticism.
Recognising Desire and Letting Go of Resistance: Longing for life before diagnosis is natural. Mindfulness helps individuals recognise this resistance, normalise change, and move toward acceptance—loosening the grip of grief.
Acknowledging That Things Will Change: Instead of resisting change, mindfulness invites softening—meeting change with awareness rather than reactivity.
Cultivating Self-Compassion: MS can trigger harsh self-judgment. Mindfulness combined with self-compassion encourages kindness and prompts the question: What do I need right now? instead of What’s wrong with me?
Supporting Identity and Transformation: MS can reshape how individuals see themselves, perhaps many times as the condition worsens. Mindfulness helps navigate shifts in identity with openness and compassion, supporting movement through common stages of:
- Rejection – Avoiding or denying the reality of MS
- Engulfment – Feeling consumed or defined by the condition
- Acceptance – Acknowledging MS as part of life without being ruled by it
- Enrichment – Finding meaning, purpose, or growth through the experience
Adapting Mindfulness for MS
Research shows that MBIs can improve physical and cognitive symptoms and enhance quality of life (Simpson et al., 2023) for PwMS. To make MBIs more accessible to PwMS, we’ve adapted our approach by offering:
- 8-week MBSR and 4-week mindfulness courses
- Both longer and shorter guided practices
- Inclusive movement practices
- MS-specific session themes
- An explicit focus on kindness and self-compassion
- Monthly drop-in sessions for course graduates to support community and practice
These adjustments help ensure mindfulness feels supportive, not overwhelming. As teachers, we’ve also drawn on ongoing mindfulness-based supervision in developing this approach.
Final Thoughts
Mindfulness can’t stop MS—but it can change how people relate to it. With compassion and awareness, PwMS can find greater emotional resilience, self-understanding and a kinder relationship with their bodies, minds, and lives. Many participants say our courses offer more than tools—they offer connection and normalisation of their experience with MS.
Phil and Yvette run four and eight-week mindfulness courses through MS_UK
References:
Sargood, Y.P., & Startin, P. H.(2025, September 24). Mindfulness and MS: Adapting MBIs for a complex journey. The Mindfulness Network. https://home.mindfulness-network.org/blog/
Simpson, R., Posa, S., Langer, L., Bruno, T., Simpson, S., Lawrence, M., Booth, J., Mercer, S. W., Feinstein, A., & Bayley, M. (2023). A systematic review and meta-analysis exploring the efficacy of mindfulness-based interventions on quality of life in people with multiple sclerosis. Journal of Neurology, 270(2), 726–745. https://doi.org/10.1007/s00415-022-11451-x